
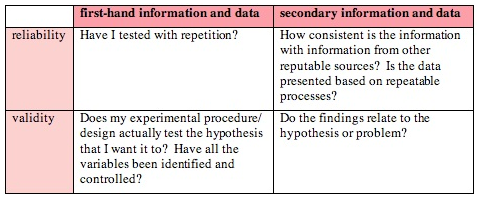
Reliability, on the other hand, relates to the ability of the measure to correctly discriminate differing levels of quality (or changes in quality) between entities. Are the timestamps in the electronic health record accurate? Can we be sure certain data fields are always populated? On a practical level we need to be sure that we accurately and consistently acquire the data used to calculate it. That is, conceptually there may be reasons why “door-to-balloon” time is or is not a good surrogate for AMI care quality perhaps there are legitimate reasons to delay angioplasty not reflected in the measure, for example. Threats to validity can be either be conceptual or practical in nature. We can demonstrate validity by correlating the measure with other, similar measures (convergent validity), by showing that it discriminates between entities we know to be different by some other metric (known-groups validity), or by having content experts weigh in on its merits (face validity).

That metric is valid as a measure of quality of AMI care as long as shorter times can be considered to consistently represent better quality. For example, measuring the time from "door-to-balloon" for an AMI patient is intended to reflect the level of quality of AMI care. Healthcare "quality" is not often directly measurable, so you're typically forced to measure surrogates you hope reflect the true underlying quality. The same is true (or should be true) for validity and reliability.Īs it relates to quality measures, validity reflects how accurately a measure represents whatever it is trying to capture.

For example, when someone on a hospital staff starts talking about the average length of stay or time to thrombolytics, you probably know that averages can be influenced by outlying data points and therefore you know to ask some more probing questions about sample size and the spread of the data from which those averages are calculated. Just like other statistical concepts, the proper use of a metric requires an understanding of what that metric does - and doesn't - represent. However, understanding the differences in these terms and what they truly represent is critical for not just those involved in measure development, but for anyone who uses a quality measure or wants to interpret its results. This is understandable: they are technical terms (i.e., jargon) and they both refer to how “good” a measure is, so it’s no surprise that the details of what falls under each category can get a little muddy.

When discussing the merits of a particular healthcare quality measure, the concepts of “validity” and “reliability” are often used interchangeably (if used at all).


 0 kommentar(er)
0 kommentar(er)
